A Silent Crisis: Why Rural Healthcare Is at a Breaking Point
In the heartlands of America, a silent emergency continues to unfold. Rural hospitals are closing. Primary care clinics are stretched thin. And healthcare workers, from physicians to frontline nurses, are burning out faster than they can be replaced. Despite their critical role in serving nearly 60 million Americans, rural health systems face an uphill battle recruiting and retaining talent. The challenges are structural, geographic, and deeply human.
This is not just a workforce shortage. It’s a full-scale care access crisis.
This is where the Mayo Clinic comes in, a name known for clinical excellence. What’s lesser known, however, is how this world-class health system is navigating and solving the very workforce dilemmas that are paralyzing rural healthcare across the U.S. With an ambitious goal to hire more than 45,000 providers and allied health professionals across the Midwest, Mayo isn’t just scaling up it’s reinventing the healthcare workforce model from the ground up.
In this blog, we discuss how Mayo Clinic addresses rural staffing challenges through bold innovations in cross-border care coordination, tele-specialist networks, burnout prevention, and continuous professional development and what health systems worldwide can learn from its strategy.
If the future of healthcare will be accessible, equitable, and resilient, a workforce model needs to be built for that.
Rural Staffing Realities: Why Traditional Models No Longer Work
Delivering quality healthcare in rural regions is not simply building hospitals or opening clinics. The core issue is people, specifically the absence of qualified professionals to staff and sustain these facilities. From the Great Plains to the Appalachian Mountains, rural communities grapple with a dangerous imbalance: soaring demand for care and an ever-shrinking supply of clinical and allied health workers.
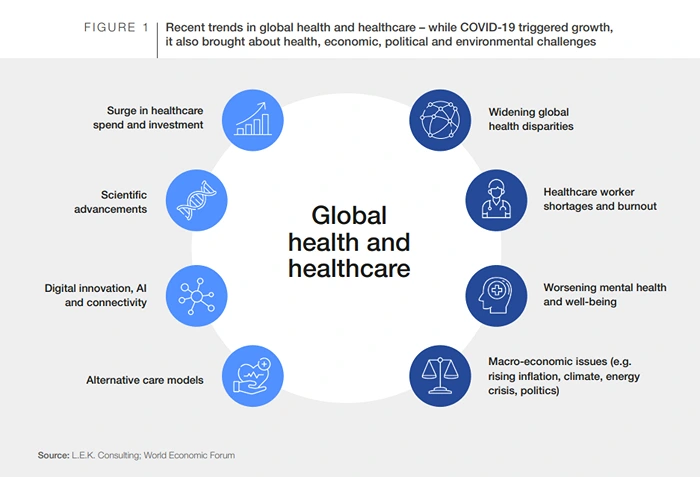
Image Source: Welcome Qatar
The Numbers Speak for Themselves
Despite making up 20% of the U.S. population, rural areas have access to just 11% of the nation’s physicians, as stated by the National Rural Health Association. What’s more alarming is that nearly two-thirds of rural hospitals struggle to recruit even one primary care provider, let alone the interdisciplinary teams required for comprehensive care delivery.
This is not just a recruitment challenge. It’s a retention crisis. New hires often leave within a few years due to professional isolation, limited resources, lack of growth opportunities, or burnout. The result? A continuous churn that weakens health outcomes and community trust.
What’s Breaking in the System
Traditional workforce models tend to assume that recruitment is primarily a matter of location and salary. Offer enough money or a relocation bonus, and someone will come. But in rural healthcare, these assumptions break down:
- Geographic isolation leads to lifestyle and family challenges that money can’t fix.
- Limited peer networks and mentorship opportunities cause professional stagnation
- Inflexible staffing models don’t accommodate personal well-being or dual-career family planning
- Delayed investment in digital infrastructure makes hybrid or remote care difficult to implement
Healthcare organizations that cling to rigid, urban-centred staffing playbooks are setting themselves up to fail in rural regions. A shift in mindset from placement to planning, local to global, and static to agile is no longer optional.
That’s where the Mayo Clinic model stands apart. It doesn’t just solve rural staffing shortages; it reimagines what a rural workforce can look like in a digital-first, globalized era.
Inside Mayo Clinic’s Workforce Blueprint: 45,000 Roles, One Vision
When most health systems consider scaling their workforce, they begin with recruiting. When the Mayo Clinic thinks about it, it starts with strategy. The difference is more than philosophical. It’s operational.
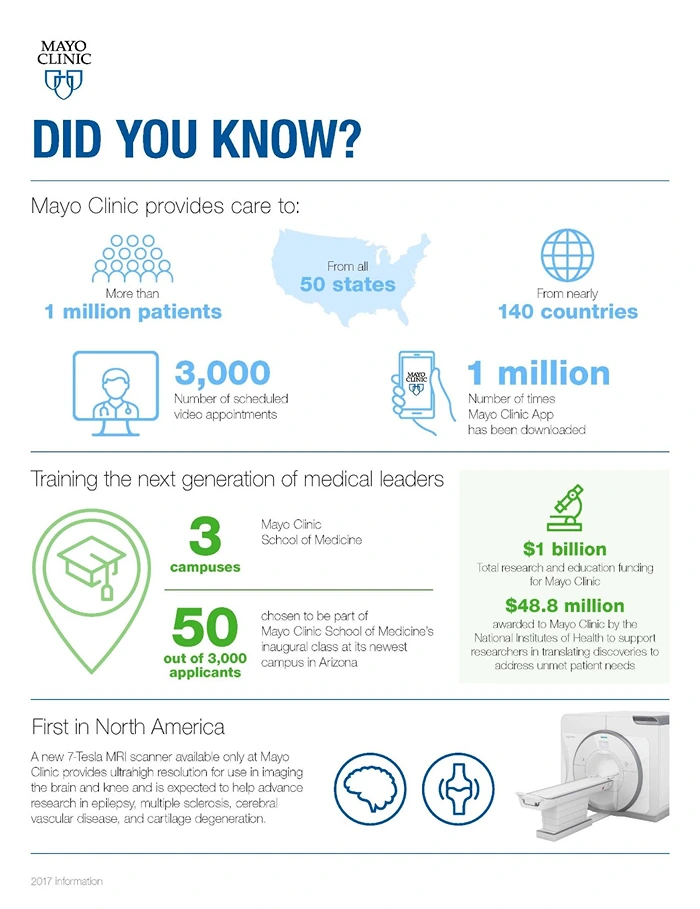
Image Source: Mayo Clinic
Facing the need to fill over 45,000 clinical and allied health roles across the Midwest and beyond, Mayo didn’t just open job postings. It reengineered its entire workforce model to deliver care across borders, disciplines, and time zones while maintaining the gold standard in patient outcomes and staff experience.
Beyond Headcount: Designing a Care-First Staffing Model
Rather than focusing solely on location-based staffing, Mayo developed a cross-border care coordination system prioritizing access, agility, and continuity. This means a doctor no longer constrains care to a location. With the proper digital infrastructure, a cardiologist in Arizona can consult on a patient case in rural Minnesota, all under Mayo’s integrated electronic health record system and coordinated protocols.
Mayo’s Vision was clear: Build a hybrid workforce that includes:
- On-site staff for core clinical functions and local patient engagement
- Remote specialists serve multiple crucial roles: filling skill deficits, increasing access to services, and providing valuable second opinions.
- Telemedicine triage teams can handle diagnostics, manage referrals, and conduct monitoring.
- Allied health professionals trained in multi-role, tech-supported care delivery
This model required deep alignment across HR, clinical operations, IT, and legal teams and an unwavering commitment to care excellence regardless of physical location.
The Mayo Operating Model: Precision Meets Scale
Mayo Clinic’s uniqueness goes beyond its reputation. It’s how it operationalizes excellence at scale:
- Centralized protocols help ensure consistent care delivery across all locations.
- Digital infrastructure enables seamless specialist collaboration
- Predictive workforce planning allows for dynamic team allocation based on demand
- Strategic hiring is driven by care gaps, not just open positions
This is not a reactive model. It’s deeply proactive. Every workforce decision at Mayo Clinic is designed to balance access, efficiency, and staff well-being, which few healthcare systems manage to get right.
That level of foresight doesn’t happen by accident. It requires data, lots of it. From market availability to talent trends, labour mobility, and skill forecasting, Mayo relies on robust insights to guide its workforce model.
That’s where solutions like JobsPikr become valuable, helping health systems decode external labour dynamics and make more intelligent, more sustainable workforce decisions.
Recruitment Reinvented: How Mayo Finds Talent Beyond Borders
Recruiting in rural America is hard enough. Recruiting for a tele-specialist network that spans state lines and sometimes continents can feel impossible. Yet the Mayo Clinic talent team has turned this challenge into a competitive edge by reengineering every step of the hiring journey around three core pillars: reach, rigour, and retention.
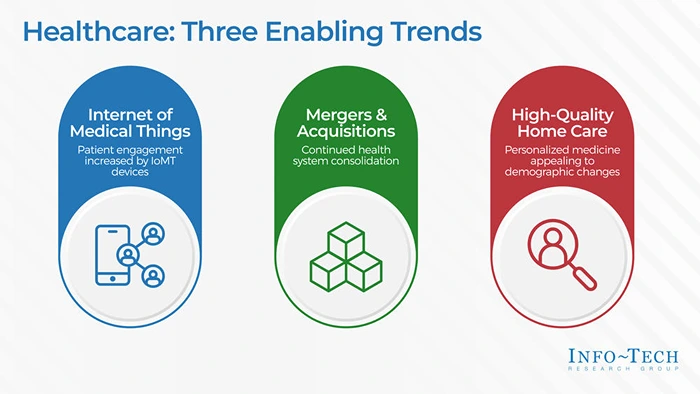
Image Source: Infotech
Casting a Truly Global Net
Traditional healthcare recruitment starts with a ZIP code and radiates outward. Mayo flips that model on its head. It pinpoints pockets of specialist density that match rural demand profiles by using detailed global talent-supply maps from licensure boards, residency databases, and external labour-market feeds. That means a shortage of endocrinologists in northern Iowa can be offset by contracting board-certified physicians in São Paulo or Manila who hold (or can quickly secure) U.S. telemedicine credentials.
Credentialing Without the Chaos
Cross-state and international credentialing is notorious for red tape. Mayo’s answer is a dedicated Provider Credentialing Hub that runs parallel to recruitment. Legal, compliance, and HR teams collaborate in real-time so licenses, malpractice coverage, and payer enrollments move forward together, often cutting onboarding timelines by 30-40 percent. The result: specialists go from “offer accepted” to “first patient consult” in weeks, not months.
Culture Fit Across Time Zones
A clinician may live 2,000 miles away but must still embody Mayo’s patient-first ethos. Interview panels, therefore, include rural site managers, virtual-care leads, and peer physicians who test for collaboration skills, digital bedside manner, and resilience.
Candidates complete simulated tele-consults using Mayo’s EHR sandbox, proving they can deliver consistent care regardless of distance or bandwidth constraints.
Data as the Recruiting Compass
Every sourcing decision is benchmarked against external market indicators, vacancy rates, salary medians, visa wait times, and burnout risk scores in feeder regions. Platforms like JobsPikr aggregate that data into a single dashboard, warning Mayo early when a speciality talent pool is tightening and helping recruiters shift focus before pipelines dry up.
The Payoff: Deeper Benches, Faster Fills
Since adopting this telemedicine workforce strategy, Mayo’s average time-to-fill for hard-to-staff rural specialties has dropped below 60 days, compared with an industry average of 120 days. More critically, rural patients gain consistent access to world-class expertise without leaving their communities.
Cross-border hiring isn’t a stop-gap; it’s a scalable blueprint for any health system facing geographic or specialty shortages. When recruitment is guided by intelligent labour data and a culture-first lens, distance stops being a liability and becomes your growth frontier.
Burnout-Proofing the Workforce: Wellness as a Systemic Strategy
Workforce planning isn’t just about hiring fast. It’s about keeping people whole. Burnout is no longer a side effect of healthcare systems, especially in rural and high-demand environments. It’s a structural threat. At the Mayo Clinic, preventing burnout is treated with the same urgency as avoiding medical errors. The logic is simple: when providers are well, patients are too.

Image Source: Focused Staffing Group
Burnout in Rural and Remote Care Isn’t an HR Issue It’s a Clinical One
Rural care professionals face unique stressors. They work in resource-constrained settings, often with limited support staff, and carry the emotional burden of serving tight-knit communities. When coupled with isolation, lack of backup, and increasing documentation demands, burnout becomes inevitable unless addressed systemically.
Mayo Clinic recognized this early. By designing care teams with redundancy, rotation, and remote support in mind, they’ve been able to distribute clinical load, reduce provider fatigue, and increase schedule flexibility, all without sacrificing quality of care.
A Multi-Layered Burnout Prevention Framework
Mayo doesn’t treat wellness as a set of perks. It embeds it across organizational layers:
- Team-Based Scheduling: Smart shift rotations that balance high-stress and low-intensity workdays
- Virtual Shadowing & Peer Support: Remote clinicians are paired with on-site partners for regular case reviews and emotional check-ins
- Built-In Recovery Time: Protected time for rest, upskilling, or research not just in theory but tracked and enforced
- Careload Algorithms: AI-backed tools assess clinician fatigue based on caseload complexity and frequency of urgent consultations
Beyond the Clinic: Well-Being in the System’s DNA
Well-being at Mayo extends beyond individuals. It’s embedded in the system’s operations, leadership KPIs, and culture:
- Department heads are trained in burnout identification and prevention.
- Exit interviews are analyzed to identify red flags related to retention and emotional well-being.
- Tele-specialist contracts include built-in mental health support provisions.
In 2024, Mayo reported a 22% decrease in provider attrition in rural markets where these burnout interventions were a remarkable achievement in a sector where burnout-induced turnover can cost systems millions annually.
At scale, this is more than just HR innovation. It’s a redefinition of what a sustainable workforce looks like. It’s a strategy that more healthcare systems must adopt if they want their providers and patients to thrive.
Continuous Professional Development: Building Skills for the Future
As medicine evolves, so must the people delivering it. New treatments, technologies, patient expectations, and regulations are transforming healthcare at a rapid pace. For the Mayo Clinic, staying ahead means making Continuous Professional Development (CPD) a strategic pillar, not just a checkbox.
This is especially crucial in rural and remote care environments, where CPD goes beyond mere education to combat the isolation and stagnation often found there. It’s about connection, confidence, and capability.

Image Source: AIHR
CPD as a Core Workforce Strategy
Many health systems treat professional development as a side offering online courses, an annual conference, and compliance training. Mayo goes far deeper. CPD is built into the staffing, scheduling, and performance frameworks from day one. Every employee, from a specialist surgeon to a rural EMT, has access to a personalized learning path that evolves with their role and regional care demands.
Integrated Learning for a Distributed Workforce
Everyone needs a shared clinical vocabulary for a tele-specialist network to function effectively. Mayo’s internal learning management system hosts scenario-based simulations, cross-functional training, and EHR-integrated modules that mirror real-world patient flows.
- New role onboarding includes remote shadowing and virtual care etiquette training
- Credential refreshers supplement specialist rotations across geographies
- Rural generalists receive continuous access to subspecialist updates, reducing unnecessary referrals
In 2023 alone, Mayo reported over 6 million learning hours logged across 35,000+ staff, directly correlating with reduced clinical errors and higher patient satisfaction ratings.
Data-Guided Upskilling: Training What the Market Demands
Here’s where external labour market intelligence becomes crucial. Instead of waiting for skill gaps to appear internally, Mayo tracks:
- Emerging demand trends in rural patient care (e.g., geriatric psychiatry, chronic pain management)
- Certification requirements in cross-border or interstate practice
- Shifting salary expectations for niche skills, indicating future competitive gaps
Solutions like JobsPikr help teams identify which skills are gaining traction across regions and which roles are trending toward scarcity. This allows Mayo to develop internal talent proactively before external market pressures mount.
Upskilling as Retention
Professional stagnation is one of the top reasons clinicians leave rural posts. Mayo’s CPD infrastructure counters that. Clinicians do not stay just because they’re paid well, but because they’re growing, evolving, and connected to a larger mission. Learning becomes both a retention lever and a mission multiplier.
As rural care demands become more complex, Mayo ensures its workforce is equipped, not just credentialed, to deliver. The rest of the healthcare world should take note.
From Reactive to Resilient: Data-Led Workforce Planning
Delayed reactions in healthcare lead to significant costs for patients, healthcare systems, and staff. Yet too many organizations still rely on outdated, reactive staffing models that leave them flat-footed in the face of changing demand. What sets Mayo Clinic apart is its investment in workforce planning as a forward-looking, data-driven discipline that aligns people, strategy, and service delivery in real-time.
Why Reactive Models Fail
When staffing decisions are driven by vacancy panic, organizations tend to:
- Hire without alignment with long-term care goals
- Overextend current teams, accelerating burnout
- Lose visibility into regional and specialty talent trends
- Ignore shifting patient care needs or demographic shifts
This approach is inefficient and unsustainable. Especially in rural and high-variance markets, healthcare organizations can’t afford to guess. They need predictive insights, not just reactive reports.
Mayo’s Strategic Workforce Planning Framework
Mayo approaches workforce planning as it systematically, proactively, and precisely approaches patient care.
- Scenario-based forecasting aids in planning for factors like seasonality, public health crises, and population growth.
- Demand modelling projects speciality needs down to the regional level
- Integrated dashboards track care volume, clinician workload, and upcoming retirements.
- Succession planning prevents critical roles from ever being unexpectedly vacant.
Everything is underpinned by data, not just internal HR metrics but real-world labour market trends.
External Market Intelligence: The Secret Weapon
Even Mayo’s internal analytics have only gone so far. To stay ahead of market shifts, they rely on external data feeds that reflect:
- Competitor hiring activity and compensation benchmarks
- Geographic migration of clinical talent
- Regional licensing or policy changes
- Skill demand surges across markets
This is where solutions like JobsPikr bring critical value, offering health systems a panoramic view of labour dynamics so they can pivot strategically, whether it’s launching a new care program, expanding tele-specialist coverage, or identifying the best location for a new rural clinic. Workforce decisions at Mayo are guided, not guessed.
Resilience by Design
Ultimately, Mayo’s data-led approach creates more than operational efficiency. It builds resilience. The ability to anticipate staffing needs, spot talent risks early, and act decisively ensures that patients are never left waiting and providers are never pushed past their limits.
In an era of accelerating change, that kind of agility is not just smart. It’s essential.

Global Lessons from a Midwest Giant
What Mayo Clinic has accomplished isn’t just a workforce win. It’s a roadmap for the future of healthcare delivery. In the face of unprecedented rural staffing shortages, evolving care demands, and rising clinician burnout, Mayo didn’t patch holes. It redesigned the foundation.
By combining cross-border care coordination, bright recruitment, burnout prevention, continuous upskilling, and data-driven workforce planning, Mayo has created a system that’s both scalable and sustainable. And while their resources may be unique, their principles are not. Any healthcare system, large or small, urban or rural, can begin to adopt these strategies with the right mindset and the right tools.
The Takeaways for Health Leaders Everywhere:
- Build hybrid care teams that combine local presence with remote expertise
- Shift from reactive hiring to proactive, scenario-based workforce planning
- Embed burnout prevention as a core operational KPI, not an HR afterthought
- Make continuous learning a retention and quality engine
- Anticipate change, don’t just react to it, by using external labour market intelligence.
In today’s healthcare economy, talent is your most limited resource and significant asset. The systems that win tomorrow won’t be those with the most job openings. They’ll have the clearest view of the talent landscape and the most innovative strategy to navigate it.
Ready to Build a Future-Ready Workforce?
JobsPikr helps healthcare systems like yours gain real-time visibility into labour market trends, recruitment bottlenecks, skill gaps, and workforce movement so you can plan smarter, hire better, and grow stronger.
Sign up today to start transforming your workforce strategy with data you can trust.